![]() Achieved
Achieved
- Publication of the Five Year Forward View
- Finalisation of the 2014-2019 PPRS agreement
- CCGs now fully operational with significant and growing commissioning responsibilities
![]() More to do
More to do
- Review of NICE processes to address accusations that it is no longer fit for purpose
- Required efficiency savings to bridge the £30billion NHS deficit
![]() The unexpected
The unexpected
- Drastic changes to the Cancer Drugs Fund operating procedures
- Barker report calling for ‘well-off retired’ to shoulder responsibility for bridging the £5bn gap in social care funding
- Cancer and A&E waiting time scandals
![]() Legacy
Legacy
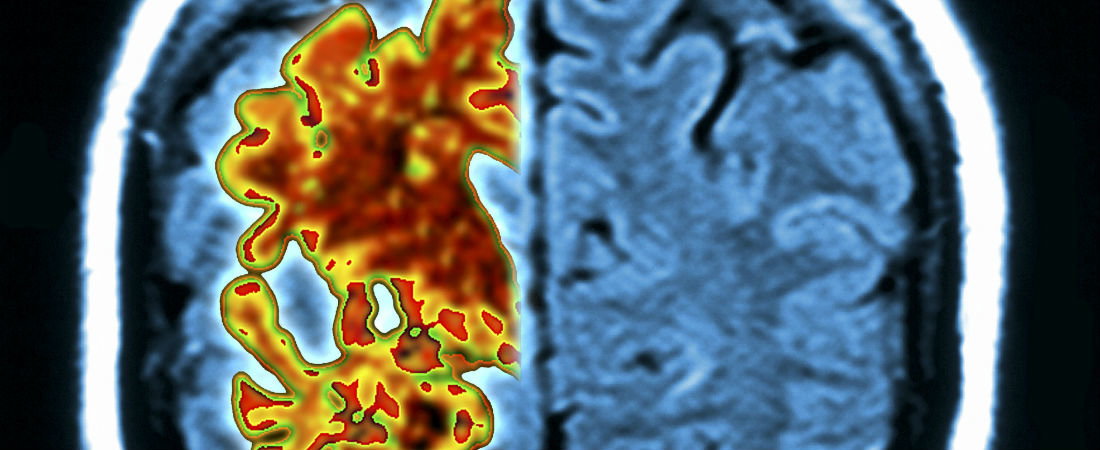
- An increasing emphasis on dementia and Alzheimer’s
- Uncertainty and controversy around the funding of cancer drugs
- Further NHS upheaval
2014 was a year of ups and downs for the NHS and the wider health and social care sector, with much change stemming from the appointment of ex-Labour adviser Simon Stevens as Chief Executive of NHS England.
His appointment demonstrates a continuing shift in responsibility away from the Department of Health.
Mr Stevens has spent his first seven months making waves both internally and externally; from scrapping and creating new directorates, to hiring old friends to head them up. There has been a middle management cull with a shift to regional leadership, potentially paving the way for his recent five-year plan.
The Five Year Forward View is being hailed as the definitive plan for the future of the NHS, with everything we can expect in the coming years alluded to in this sizeable document. The more exciting headlines include an emphasis on the role of technology; new care models; the rise of multispeciality providers and small hospitals; prevention, and empowering patients to take responsibility for their own care.
Arguably the plan’s key role is to outline the savings required to bridge the £30billion deficit the NHS is facing. However, what appears to be another statement of planned bureaucracy could be seen as the start of Mr Stevens’s ‘big revolution’, with the upheaval to come. We should expect a pro-competition stance to feature in coming years, despite no official mention of the ‘c-word’. Whatever happens, we know that pressures on NHS resources will only continue into 2015.
The 2014 Pharmaceutical Price Regulation Scheme (PPRS) has also been a source of controversy with the battle between NICE and the pharma industry raging on. There has been a clear split between those that believe rejecting new drugs on cost grounds is the right thing to do, and those that believe these decisions are stifling innovation. Whilst pharma insist that price should no longer play a part in NICE’s assessment of new drugs due to the hefty rebate system, NICE has continued to press on pricing, becoming increasingly vocal.
The Department of Health, meanwhile, announced controversial changes to the operating procedure for the Cancer Drugs Fund, effectively duplicating the role of NICE by introducing an assessment of drugs’suitability based on price. Patient groups and industry have been up in arms and we can expect an ongoing and robust dialogue on the issue. While it is clear that the CDF is one sticking plaster that can’t last for ever, it remains to be seen if an agreement can be reached on funding of future cancer care.